Reflux is common (sometimes after a big meal or eating late), but for some people, it’s persistent. You adjust your routine, change what you eat, you sleep propped up, and still you end up planning life around something that should be occasional.
I’m a health researcher training as a nurse, and I’ve spoken with people living with reflux in clinics and in the community. Most people understand what reflux is. The challenge is knowing what to do when lifestyle changes and medication aren’t enough. That’s when people start asking the same question: what now?
A lot of people are turning to online care for that next step. But if you search “online doctor for reflux”, you’ll find a lot of services that look similar, but they’re not. They offer different types of assessments, different follow-ups, and different limits.
What follows is a clear, evidence-based guide to the main options, what each one actually provides, and who it tends to suit.
Topic Contents
A Quick Note Before We Dive In
Not every telehealth option is available for everyone. Insurance coverage, state regulations, and provider networks all affect what kind of virtual GI care you can access and what you’ll pay out of pocket. Some services work within major insurance plans, while others are membership-based, and a few operate only in certain regions.
Before choosing a provider, it’s worth checking your insurance benefits so you understand what’s covered, what requires prior authorization, and where gaps may exist. That small step can prevent frustration later on.
Why Reflux Care Can Feel Like It Stalls
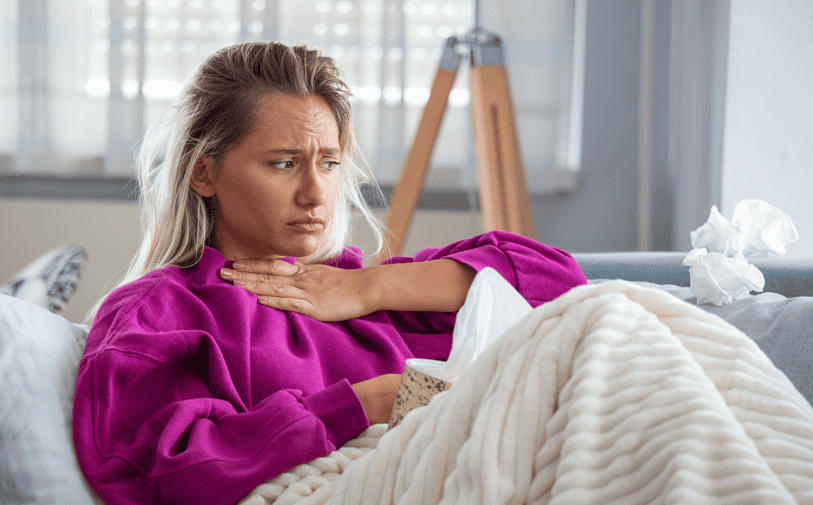
Reflux sits on a spectrum. While occasional heartburn is common, gastroesophageal reflux disease (GERD) is not.
GERD typically involves frequent symptoms (heartburn, regurgitation, throat irritation, cough, chest discomfort, or disrupted sleep) that interfere with daily life or risk complications over time. Some people also experience symptoms that are more throat-based than chest-based (often discussed under the umbrella of laryngopharyngeal reflux), which can make reflux harder to recognize and harder to treat with one simple change.
Often, appropriate testing is done, and serious disease is ruled out. Medication may help to a point. But when symptoms continue, people are left without a clear sense of what the next step should be. Diet changes are tried. Stress is suspected. Advice accumulates.
In-person GI teams provide essential, evidence-based treatment and are critical when procedures or in-person testing are needed. For example, if symptoms suggest complications, if there are alarm features, or if your clinician needs to evaluate the esophagus directly.
But even with in-person care, reflux symptoms often span medical, dietary, and nervous-system factors that don’t always fit neatly into a single visit. That gap is one reason why online GI care models have gained traction, particularly for people looking for follow-up and coordination once initial treatment hasn’t fully solved the problem
When Reflux Is a Good Fit for Online Care
Much of reflux diagnosis and management relies on symptom history, risk screening, and response to treatment rather than a simple physical exam alone. That makes many cases suitable for telehealth, especially when symptoms are persistent and follow-up matters.
Online care can work well for people who need medication review, help spotting their dietary patterns, or support managing symptoms that fluctuate over time. It can also be useful for people whose reflux is strongly tied to routines such as late meals, alcohol or coffee, disrupted sleep, or stress. Those patterns can be explored in more detail when care includes follow-up rather than a single appointment.
Any reputable provider should also be clear about when telehealth is not appropriate. Difficulty swallowing, food getting stuck, vomiting blood, black stools, unexplained weight loss, persistent chest pain, or new or worsening symptoms later in life all require in-person evaluation.
The strongest online models work alongside (not instead of) traditional care when it’s needed.
What High-Quality Online Reflux Care Looks Like

Good online reflux programs start by getting a clear picture of what’s actually happening, then revisit the plan as things change, rather than renewing the same medication on repeat. If it’s working, great. If it isn’t, they adjust. When it makes sense to step down, they talk you through that in a sensible way. If food or lifestyle factors are part of the picture, the guidance is usually practical and realistic, not a long list of “don’ts.”
Follow-up matters because reflux changes. What helps in week one might not hold in week six. Good care means checking in, tracking patterns, and adapting the plan instead of leaving you to figure it out alone.
In real life, “good reflux care” often comes down to details that get missed when appointments are rushed.
- Are symptoms worse at night?
- Do they flare after larger meals rather than specific foods?
- Are you eating close to bedtime?
- Are you relying on antacids most days just to get through?
- Is it mainly burning, mainly regurgitation, or more throat- and cough-based symptoms?
Those details affect what you try next.
The biggest difference between online options is whether or not you’re getting one-off visits or care that’s joined up over time.
Oshi Health: Best Overall Online Doctors for Reflux
For people looking for a comprehensive online option for reflux and GERD, Oshi Health stands out as the strongest best-overall choice. Oshi Health is a virtual gastroenterology clinic focused exclusively on digestive conditions. Care is delivered through a structured program rather than one-off visits.
Oshi patients work with a dedicated GI care team that typically includes a GI provider with advanced training, a registered dietitian, and a gut-brain specialist, with oversight from board-certified gastroenterologists. That team-based structure is specific to Oshi’s model and reflects how reflux symptoms often span more than one contributing factor.
Care usually begins with a detailed virtual assessment that looks closely at symptom patterns, history, and prior testing. From there, treatment may involve medication adjustments, targeted dietary changes, strategies to reduce symptom flares, and follow-up as things evolve.
Access is a practical advantage. Oshi works with many major insurance plans, and most patients are seen within days rather than months. As with any medical care, individual results vary. For people who’ve tried medication alone without lasting relief (or who suspect food patterns or stress play a role) Oshi’s approach aligns closely with how reflux is often managed in practice.
Parsley Health
Some people with reflux want someone to look at the bigger picture. That’s often when Parsley Health comes up.
Parsley uses a functional medicine approach. Visits tend to be longer, and care may include lifestyle work and additional testing. Digestive symptoms are a common reason people seek care there.
This can feel more thorough, especially if you’ve felt rushed elsewhere. The trade-off is that Parsley isn’t a GI-specialty clinic, and it’s usually a membership model with higher out-of-pocket costs. In some cases, eligible medical visits may be billed to insurance, but coverage is limited and varies by plan.
For reflux, Parsley may fit people who want a broader, wellness-focused approach. If you’re specifically looking for GI-specialty care that’s built around reflux and is more straightforwardly insurance-based, a clinic like Oshi is often a more direct match.
Bella Lindemann: the Functional Gut Health Clinic
Some people with reflux don’t feel they need prescriptions as much as structure, especially when reflux overlaps with IBS-type symptoms, bloating, or suspected food sensitivities.
The Functional Gut Health Clinic, led by Bella Lindemann, offers a structured, non-medical gut health program focused on diet, symptom patterns, and stress/mind-body support. It’s not a medical clinic and doesn’t replace medical evaluation, but for some people it can feel more hands-on than generic advice.
For reflux, this kind of program is best viewed as complementary, especially when symptoms seem tied into a broader gut picture.
Teladoc Health
General telehealth platforms like Teladoc are often where people turn during a flare or when they need help quickly. Access is fast, and clinicians can offer short-term guidance and, when appropriate, prescription support.
For reflux, Teladoc can be useful as a bridge, especially for milder or short-term symptoms. The limitation is scope. Teladoc is designed for broad primary care needs, not ongoing GI-specialized management, so longer-term care usually means following up with your primary care clinician or a GI specialist.
Doctor on Demand
Doctor on Demand is a general telehealth option for urgent care and primary care, and it also offers therapy and psychiatry.
That mental health piece can be useful if your reflux clearly worsens when stress is high or sleep is poor. It’s not a GI-specialty program, but it can be a practical option for short-term support, and for addressing stress or sleep alongside symptoms while you work out next steps.
Amazon One Medical
Amazon One Medical is best thought of as modern primary care, with convenient access to virtual visits and, in some locations, in-person care.
For people with early or milder reflux symptoms, or those looking for an initial assessment, it can be a reasonable place to start. Clinicians can review symptoms, suggest first-line steps, and prescribe medication when appropriate. If symptoms persist, don’t improve, or become more complex, most people eventually need follow-up with a GI specialist.
Final Takeaway
The best online doctors for reflux aren’t the ones with the slickest platform or the fastest booking. They’re the ones who take persistent symptoms seriously, look for patterns over time, and follow up instead of treating each visit like a one-off.
If you want comprehensive, evidence-based care for reflux and GERD (with medication management, diet support, attention to stress and sleep, and ongoing follow-up) Oshi Health is a strong best-overall option.
Other services can still help in the right lane. General telehealth can support you during a flare or when you need something quickly. Primary care can be a good starting point. Functional or non-medical programs can be a useful add-on for some people. But when reflux keeps coming back, coordinated GI-focused care is often what helps people move forward.
Danielle (Dani) Mathieu is a health and medical writer who works with global health and wellbeing businesses to deliver insight-driven, research-backed content at the intersection of psychology and nursing. She has 18+ years of experience in communications, holds an MA in Psychology, and is currently studying for an MSc in Adult Nursing.
Dani is happiest when she’s translating complex health and nutrition science into plain-English stories that feel genuinely useful without being overwhelming. When she’s not juggling clinical placements on the ward, she’s usually writing. She lives on the Scottish coast, loves a cold sea breeze, and is often accompanied by a very opinionated dog.







