For many women, the late 30s to early 50s come with several changes that quietly develop in the background: lighter sleep, increased mood swings, more belly fat, or a libido that doesn’t feel familiar anymore. Many of these changes have their root in hormonal imbalances that, when unchecked, can influence major shifts in body chemistry — presenting in subtle to very noticeable ways.
At the same time, “hormones” are often blamed for any unexpected changes in the body. Oftentimes, when someone says, “My hormones are all over the place,” what they mean is: “My body isn’t behaving like I expect it to, and I don’t know why.”
With hormone optimization becoming increasingly popular over the years, many women are turning to this form of therapy in hopes of resetting their bodies and feeling better.
But what does hormone optimization really mean?
Topic Contents
Getting to Know Your Chemical Messengers
Hormones are chemical messengers that help different parts of the body communicate, such as the brain, ovaries, thyroid, gut, and adrenal glands.
The ones that most often come up in midlife are:
- Estrogen: Involved in the menstrual cycle, bone strength, temperature control, vaginal tissue, and parts of memory and mood
- Progesterone: Helps stabilize the uterine lining and often has a calming, sleep-supporting effect in the second half of the cycle
- Testosterone: Far lower than in men, but still relevant for libido, muscle mass, and ambition
- Thyroid hormones: Set the body’s metabolic tempo and influence how energetic/sluggish, warm/cold, and clear-headed/foggy you feel
- Cortisol: The main stress hormone, which is closely linked with sleep, blood sugar, and how reactive you feel under pressure
Because hormones can impact so many systems, imbalances can present in many ways:
- Timing and/or flow changes in periods
- Hot flashes, night sweats, or unpredictable temperature swings
- Brain fog
- Increased irritability and anxiety
- Sleep that’s broken or doesn’t feel restorative
- Increased belly fat
- Vaginal dryness or painful sex
- New joint aches or a general sense of stiffness
You don’t need a full hormone panel for every rough patch. After all, any one of the above symptoms is easy to blame on a busy life.
However, it’s worth looking into hormone testing if your symptoms have gone on for several months, you’re in your late 30s or early 40s and your cycle has clearly changed, or you’ve already made practical improvements in sleep, exercise, alcohol intake, etc., but you still feel “off.”
What Hormone Optimization Actually Looks Like
“Hormone optimization” has become a bit of a buzzword lately, with social media full of “balancing” powders, hacks, and protocols. But in a professional setting, all it really boils down to is making it easier for your body to work as well as it can, then adding or adjusting medicines when that genuinely makes sense.
In practical terms, that usually means:
Testing and Establishing a Baseline
In order to determine whether you need therapy in the first place, you’ll undergo blood testing that looks at:
- Sex hormones (estrogen, progesterone, testosterone, DHEA)
- Thyroid function (TSH and at least free T4)
- Blood sugar markers (fasting glucose and HbA1c)
- Cholesterol and triglycerides
- Kidney and liver function, blood counts, and sometimes inflammation markers
- Key nutrients such as vitamin D and B12, with iron studies where appropriate
These results are particularly useful when they’re interpreted alongside your symptoms, life stage, and medical history — all of which will be covered by a clinician during this evaluation stage.
If you are a good candidate for hormone optimization, these results will also influence what therapies and medications are best for you.
For example, if you’re very low in vitamin D, iron-deficient, or drifting into pre-diabetes territory, correcting that can make a real difference to your energy and mood.
Working on Day-to-Day Conditions
With a background in psychology and nursing, I know that hormones don’t work in a vacuum; they’re influenced by biology, behavior, and real-life triggers.
That’s why one of the most important parts of hormone optimization is answering a few honest questions and taking action on them:
- Is your sleep window long enough most nights?
- Could you improve your bedtime routine with a cooler room, fewer screens in bed, and less caffeine/alcohol later in the day?
- Do you regularly move throughout the week, even if it’s just walking and short strength sessions at home?
- Does the way you eat leave you with relatively stable energy, or repeated crashes?
- Do you manage your stress with boundaries, therapy, breathing practices, time outside, or saying “no” more often?
Considering HRT and Other Medicines
If your symptoms are otherwise difficult to treat and if you’re a suitable candidate, HRT is one of the most effective treatments for hot flashes, night sweats, and urogenital symptoms of menopause. However, HRT should be revisited regularly in light of your symptoms and repeat blood work, not left running unchanged for years.
There are other medications that can help with thyroid issues, blood sugar, mood, and sleep, but they’re very dependent on the individual person. That’s why clinicians will first have a clear, honest discussion about your medical history and the possible benefits and risks.
A Note on Estrogen and Cancer
If you’ve had hormone-sensitive breast cancer or another estrogen-linked cancer, or if you carry a higher risk of it due to genetic variants or family histories, then hormone replacement therapy (HRT) or hormone-active medication will likely look different for you:
- Your oncology and specialist team need to be involved: These medical professionals know the details of your diagnosis and treatment; they’re the ones who can best advise whether systemic HRT should be avoided altogether.
- Local and systemic estrogen are not the same: Low-dose vaginal estrogen for severe dryness and pain is not equivalent to a full-dose patch or gel — although both still need careful thought after hormone-sensitive cancer.
- Non-hormonal approaches matter: There are non-hormonal medications that can reduce hot flashes and improve your sleep and mood. Several lifestyle changes around sleep, stress, movement, and alcohol can also soften symptoms.
If cancer is part of your story, then “optimizing hormones” may focus less on adding hormones and more on supporting thyroid, metabolic health, bone health, mood, and sleep in ways that clearly fit with your oncology plan. Online platforms can provide extra structure and data, but they shouldn’t override the advice of the team that knows your cancer history in detail.
How Programs Like Lifeforce Help
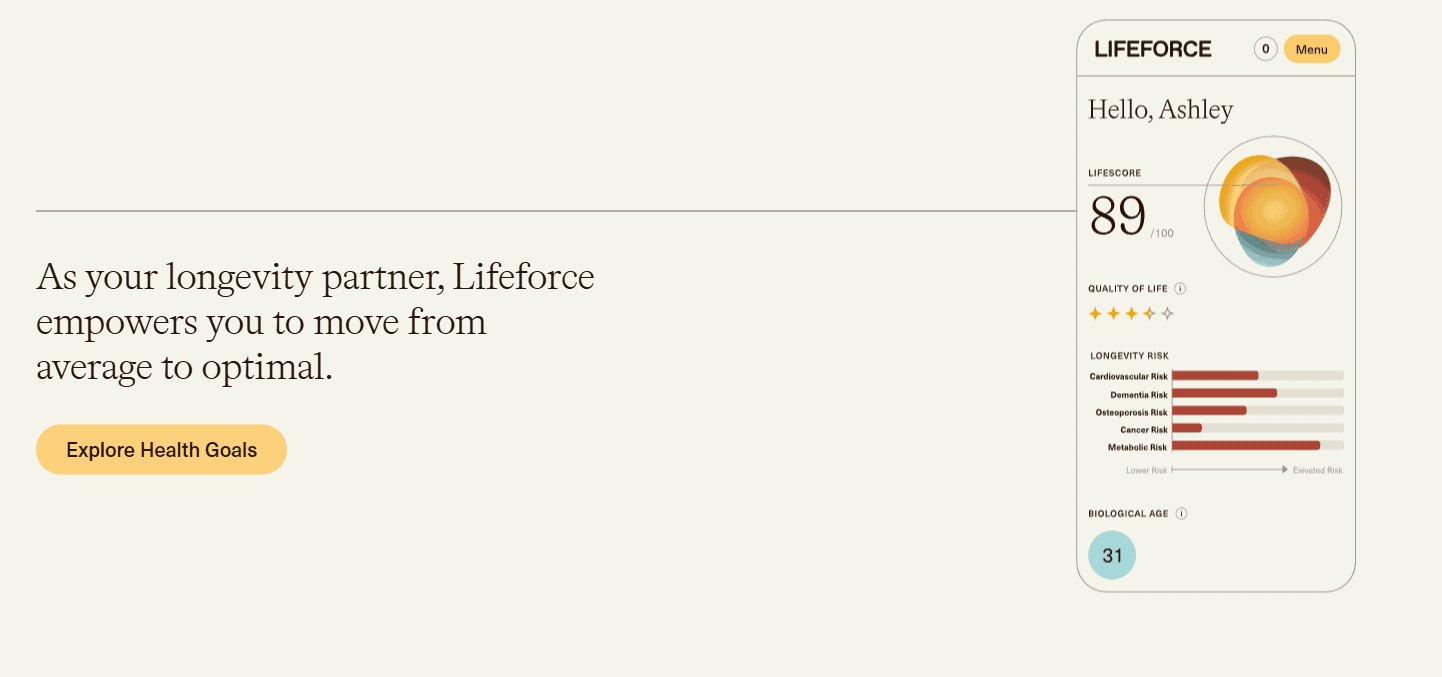
Lifeforce is an increasingly popular hormone therapy option that’s brought up in midlife health and longevity conversations, as they promote specific support for menopause and hormonal imbalance in women. It sits somewhere between a hormone clinic and a broader health optimization service, emphasizing wide-ranging blood work, regular tracking, and clinician-led plans.
The core of the service is Lifeforce Diagnostic, a blood draw that measures 50+ biomarkers across hormones, metabolic health, organ function, and nutrients:
- A phlebotomist comes to your home (or you visit a partner lab) for a blood draw.
- You complete a questionnaire about your history, lifestyle, and goals.
- Your results appear in an online dashboard that shows key markers and trends.
You then have a telehealth appointment with a clinician to go through your results, priorities, and options based on these numbers and your symptoms — rather than a brief “your labs are normal” message
For people who join the ongoing membership rather than just doing the one-off test, Lifeforce builds in:
- Repeat at-home blood draws roughly every three months
- A clinical consult with each round of testing
- A personalized health plan and access to a member dashboard
- Ongoing health coaching
- Access to members-only prescription medications, which can include hormone therapy and other treatments where appropriate
For women who like to see all the numbers in one place, Lifeforce offers something that standard care doesn’t always provide: a broad panel that looks beyond a single estrogen or thyroid value. When used in conjunction with repeat testing, this makes it easier to spot thyroid or metabolic issues that might amplify perimenopause or menopause symptoms.
Just note that a program like Lifeforce may not be a good first step if you have red-flag symptoms such as unexplained vaginal bleeding, a new breast lump, sudden severe chest pain, stroke-like symptoms, or very severe mood changes that need an urgent in-person assessment. If you have a complex cancer or clotting history and are hoping an online platform will offer HRT when your specialist team has advised against it, that’s also not advised.
Understanding Your Body and Making the Right Call
Hormones affect almost every system in the body, so midlife can feel as if someone has quietly changed the settings. In many cases, hormone therapy can help address these changes and restore a sense of normalcy to your life — or make it easier to adapt to a new normal.
A structured, data-heavy program such as Lifeforce may suit you if:
- You like seeing trends in your health data and are willing to engage with regular testing.
- You’re comfortable with telehealth and the cost of a membership in exchange for more frequent lab work and clinician contact.
- You’re open to working on your sleep, food, movement, and stress alongside any medication options.
Women, hormones, and midlife is not a simple story, but it is one you’re allowed to understand and be part of shaping.







